UCalgary research recommends nerve blocks to treat migraines
Posted Dec 5, 2025 3:17 pm.
Last Updated Dec 6, 2025 9:53 am.
Severe migraines are sending many Calgarians to hospital emergency rooms in search of relief — and now, new research suggests a simple injection could provide faster, longer-lasting results.
Doctors say Calgary’s altitude, frequent Chinook winds, and even genetic factors may make residents more prone to migraines. For those living with the condition, coping often means turning to whatever works in the moment.
“I go for physiotherapy, and it releases my muscles,” said one local sufferer.
Another explained, “I’m usually using things like Robaxin and muscle relaxers.”
For some, relief comes from family support: “My wife suffers from migraine pain, and since she just moved here, she can’t see a doctor yet. The only option we have is for me to massage her head.”
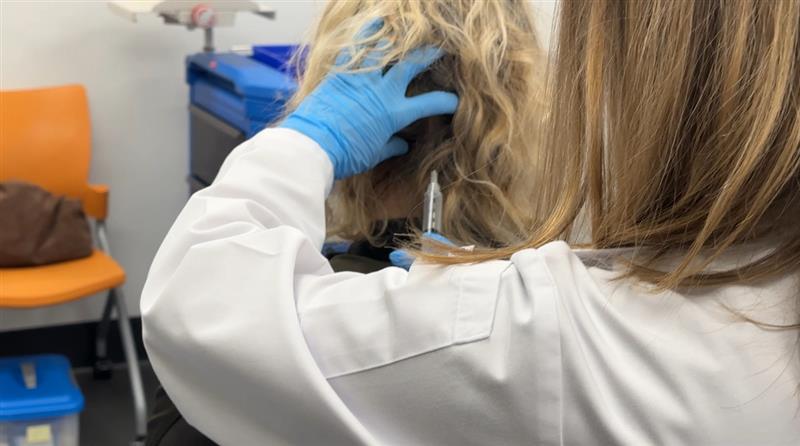
But a newly published study from the University of Calgary offers hope. Neurologist Dr. Serena Orr says an occipital nerve block — a quick injection at the base of the skull — can safely and effectively reduce migraine pain.
The findings are published in “Headache: The Journal of Head and Face Pain” and update the 2016 guidelines of the American Headache Society for the management of migraine attacks in emergency departments.
The update reviewed 26 studies from the past nine years that met the criteria involving migraines and visits to emergency departments to bring the treatment recommendations up to date.
“We do injections in two to four areas at the back of the head,” Orr explained. “Within a few minutes, the back of the head goes numb. And so the relief more broadly outside of the back of the head can happen within anywhere from 30 minutes to two hours, which is what we see in the clinical trials.”
Side effects are generally mild, and many migraine sufferers say they would be willing to try it.
“Most of my headaches start from the back of my neck into my head, so I’d give it a try,” said one.
Another added, “If I had acute migraines, I would definitely consider it.”
Orr is also studying newer, less invasive treatments such as remote electrical neuromodulation, which could one day be used in ERs. While nerve blocks have been available for years, not all emergency staff are trained or comfortable administering anesthetic-based procedures.
Researchers hope new guidelines will encourage more hospitals to adopt nerve blocks as a frontline option for migraine patients — provided proper training is in place.
With files from The Canadian Press








